VIVO Pathophysiology
Erythropoietin
Erythopoietin is a protein hormone essential to production of red blood cells (erythrocytes), which themselves deliver oxygen to all tissues in the body. This hormone is synthesized in the kidney and its secretion is regulated by the amount of oxygen delivered to that organ. Erythropoietin was one of the first drugs produced through recombinant DNA technology and is widely used in conditions where red blood cell production is deficient.
Structure and Synthesis
Erythropoietin is a small (~30 kDa) glycoprotein structurally similar to growth hormone. In the fetus, it is synthesized in the liver, but production later switches almost exclusively to the kidney. Within the kidney, erythropoietin is produced by interstitial fibroblast-like cells that surround the renal tubules.
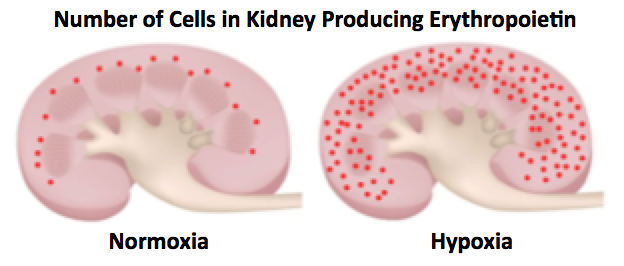
When blood oxygen concentration is normal (normoxia), synthesis of erythropoietin occurs in scattered cells located predominantly in the inner cortex, but under conditions when blood oxygen is deficient (hypoxia), interstitial cells within almost all zones of the kidney begin to produce the hormone. This is an interesting concept - increased production of erythropoietin is due to an increase in the number of cells that produce it rather than an increase in the level of synthesis by particular endocrine cells. Expression of erythropoietin in individual cells is regulated essentially an on/off switch rather than via increase/decrease.
Under hypoxic conditions, for example with severe anemia, the kidneys can increase production of erythropoietin more than 100 fold over normal.
The erythropoietin receptor is a dimer of a transmembrane protein expressed on the cell surface of target cells. Binding of erythropoietin to its receptor activates an intracellular kinase that phosphorylates the receptor, changing its conformation; signal transduction with cells is terminated when the receptor is dephosphorylated and the hormone-receptor complex is internalized.
Physiological Effects of Erythropoietin
Erythropoietin is essential to the production of red blood cells because it is required for survival, proliferation, and differentiation of erythroid progenitor cells in the bone marrow. In the later stages of erythrocyte differentiation, the receptor for erythropoietin is downregulated and the hormone no longer necessary for cell survival.
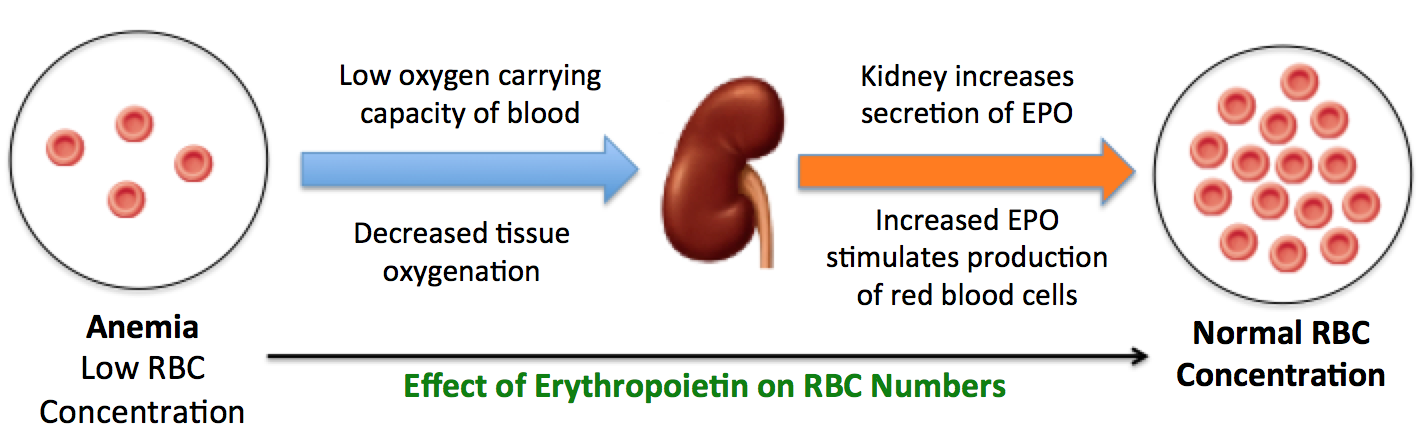
Red blood cells deliver oxygen to all tissues and when red cell numbers are reduced or abnormal - a condition called anemia - tissues are deprived of oxygen. Anemia can result from a broad range of problems, for example from hemorrhage, destruction of red cells due to autoimmunity, or interference with cell production associated with cancer chemotherapy. As depicted below, anemia leads to hypoxia within the kidney, which triggers additional interstitial cells there to start secreting erythropoietin. Increased secretion of erythropoietin enhances and accelerates the production of new red blood cells from their progenitors.
In addition to its effect on red blood cell production in the bone marrow, erythropoietin has been implicated in a number of other cellular effects in vasculature, heart, and nervous system. The importance of these other influences is poorly understood.
Disease States
Erythropoietin is necessary for life in vertebrates. Mice that are homozygous for deletions of the erythropoietin gene die early in gestation from severe anemia.
A common cause of erythropoietin deficiency is chronic kidney disease. When the kidneys are damaged, their ability to produce erythropoietin is compromised and anemia ensues. The anemia associated with chronic kidney disease can be alleviated by treatment with erythropoietin. Such treatment is also valuable in a number of other types of disease associated with deficits in red blood cells production.
References and Reviews
- Kelkmann W. Physiology and pharmacology of erythropoietin. Transfus Med Hemother 2013; 40:302–309.
- Kurtz A. Endocrine functions of the renal interstitium. Eur J Physiol 2017; DOI 10.1007/s00424-017-2008-9.
Updated 2018. Send comments to Richard.Bowen@colostate.edu
